Pratyaya Deep Bhattacherjee2, Dipanjan Saha2, Soumen Kumar Das2, Ratna Dey3, Malobika Ghosh3, Iti Dutta3, Madan Sarma3, Parthasarathi Bhattacharyya1.
1Consultant, 2Research fellow, 3 Research Assistant. Institute of Pulmocare and Research, Kolkata, India.
Abstract
Background: Treatment of Class III pulmonary hypertension that can affect the oxygenation and quality of life may be worthwhile.
Objective: To identify class III pulmonary hypertension in a tertiary pulmonary OPD practice and observe the effect of treating them with sildenafil on defined indications.
Methods: The presence of pulmonary hypertension was diagnosed on a composite clinico-radio-echocardiographic criteria and the etiological factors were identified using an evaluation algorithm in a referral OPD services. Concomitant to the optimum treatment of their underlying etiological conditions, the WHO functional class III and IV patients from varied etiologies were treated with sildenafil on a real world protocol. The quality of life measured with CAT (COPD assessment test) score, and the resting arterial oxygen saturation were noted at the beginning and after 3 months of sildenafil therapy with documentation of the adverse and serious adverse events.
Results: 81 patients (mean age 62.43±10.17 years) from different etiologies have been recorded to have documented follow up on sildenafil. COPD (35.7%), past history of tuberculosis (21%), indeterminate etiology (13.5%), DPLD (13.5%), and asthma (11%) remain the major causes of pulmonary hypertension. There has been universal improvement across the different causes with the mean CAT score reducing from 15.33±5.52 to 13.01±5.79 (p=0.004) and the mean arterial oxygen saturation improving from 94.6±2.90 to 95.05±3.15 percent. The improvement in CAT was significant for COPD (p=0.03, n=29)
Conclusion: the causes of Class III PH looks different than known and the patients show improvement in quality of life following sildenafil therapy.
KEY WORDS: pulmonary hypertension, pulmonary artery pressure, quality of life, CAT (The Pulmo -Face, 2014; 14:1, 5-9 )
Address of correspondence: Dr. Parthasarathi Bhattacharyya, Institute of Pulmocare and Research, CB-16, Sector-1, Salt Lake, Kolkata- 700 064, India, Email: parthachest@yahoo.com
ABBREVIATIONS:
PH – pulmonary hypertension
OPD – out patient department
PDE5 – phosphodiestyerase-5
QoL – quality of life
COPD – chronic obstructive pulmonary disease
DPLD – diffuse parenchymal lung disease
OSA – obstructive sleep apnoea
CAT – COPD assessment test
RHC – right heart catheterization
HRCT – high resolution computed tomography
CPAP – continuous positive airway pressure
PA – pulmonary artery
PTB – pulmonary tuberculosis
SD – standard deviation
BD – broncho dilatation
FVC – forced vital capacity
FEV1 – forced expiratory volume in 1 second
AE – adverse event
SAE – serious adverse event
PA view – posterio-anterior view
PAP – pulmonary artery pressure
INTRODUCTION:
Pulmonary hypertension (PH) is not uncommon in different respiratory disorders including OSA(1,2). It affects the QoL adversely. (3) The diagnosis of PH appears greatly restricted in the developing world for lack of RHC as recommended by the guidelines,(4,5) and thus, possibly, a huge number of patients are deprived of the likely beneficial effects of anti PH treatment. Amidst scanty data from the Indian subcontinent, the actual prevalence of PH attending pulmonologists is not negligible. (6) The existing guidelines are not very clear to recommend the medical therapy of class III PH from different causes. Here, we present our initial experience of a real world study of looking at the effect of sildenafil on selected class III PH patients in a pulmonologist's day to day practice without adopting RHC.
METHODS:
The study was performed in a referral pulmonary OPD at Kolkata, India observing a real world protocol been approved by the institutional ethics committee. The method included a) Selection and confirmation of class III PH, b) selection of candidates for anti PH therapy and prescription of sildenafil, and c) observation of the efficacy of treatment in terms of QoL (quality of life) and change in oxygenation (arterial oxygen saturation) with concomitant recording of the adverse and the serious adverse events.
a) Selection and confirmation of PH: The diagnosis of pulmonary hypertension was made at the institute following an indigenous clinic-radio-echocerdigraphic criteria (without doing right heart catheterization).
The diagnostic approach was initiated with suspicion of PH been done from one or more of the following as i) History of dyspnoea, often disproportionately severe, with or without syncope or chest pain, ii) resting low arterial saturation at room air, iii) disproportionate reduction of saturation on exertion with no other obvious explanation, and iv) features of corpulmonale and the cardiac auscultation revealing accentuated second heart sound from pulmonary valve closure with or without pulmonary systolic murmur. The patients were subsequently evaluated with chest x-ray (PA view) and HRCT chest for signs of PH. (7, 8, 9, 10) Once PH-suggestive or PH-specific signs are present these subjects were subjected to doppler and tissue doppler echocardiography following a prescribed protocol by a single echocardiographist. The PH determinant value in echocardiography was the calculated pulmonary artery systolic pressure of ≥ 40 mm of Hg. The echocardiographic exercise included looking for the tricuspid jet velocity (greater than 2.8 m/s) and tricuspid insufficiency pressure gradient (greater than 31 mm mercury) along with measurement of the tricuspid annular plane systolic excursion (TAPASE), right ventricular outflow tract velocity profiles and different pulmonary flow indices as acceleration time and pre-ejection periods with measurement of tricuspid annular velocity (Tei) and the right ventricular ejection time based on the on this velocity profiles.
The patients satisfying the clinical, radiological (both x-ray and HRCT chest), and echocardiographic criteria favoring the presence of PH were stamped as having PH and were included for the therapeutic trial. We followed an indigenous algorithm for simultaneous diagnosis of the etiology (figure 1). In case of more than one etiology been present, the predominant one has been noted and in cases where a definite etiological diagnosis cannot be made, the patient had been placed in an etiologically 'indeterminate' group
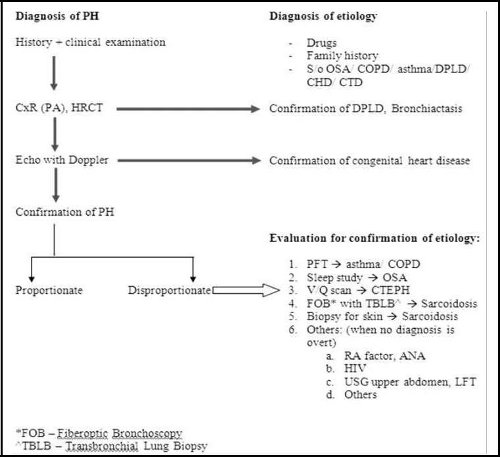
Figure 1: showing the algorithm been observed by the institute to diagnose PH and determine the etiologies.
b) Selection of the subjects for treatment: The anti-PH therapy was considered after all the subjects were treated adequately for their underlying disease under the given circumstances. The COPD patients were treated with standard COPD pharmacotherapy, home oxygen (whenever indicated), and the best possible rehabilitation measures under the logistic situations. Similarly, the DPLD patients were given treatment as per recommendations with or without home oxygen supplementation and the OSA sufferers were put on CPAP/ auto CPAP therapy. They were considered treatment with sildenafil in addition to the treatment of underlying disease if they continue to show one or more of the following despite the optimal possible treatment of the underlying conditions as (i) a functional status of class III or IV (WHO classification). (11) (ii) poor quality of life with compromised life style, (iii) Baseline resting oxygen saturation <92% at room air in at least two different occasions, and (iv) desaturation ≥ 3% on walking 15 yards or less in the consultation office.
The patients with overt right ventricular failure or functional class IV status with resting saturation being less than 90 percent with PH been quite evident were directly taken up for PH therapy PH therapy with sildenafil with concomitant optimization of the treatment for the etiology with or without advice of hospitalization.
The patients with history of any sure or suspected history of sildenafil toxicity or intolerance or allergy to the agent and the patients on concomitant use of nitroglycerines were excluded. Any patient with pregnancy, lactation, or having any significant systemic disease was excluded from the study at the beginning.
All the patients were discussed about the potential and known side effects of sildenafil and requested to report any suspected or sure side effects while on treatment. Apart, telephonic enquiries were done to all after 15 days of starting the treatment for any intolerance /adverse events. The dose to start with was 10 mg thrice daily and it was hiked to 20 mg thrice a day on tolerance after 3 to 7 days.
c) Observation of the efficacy of treatment: The quality of life was assessed at the initiation and after 12 weeks of treatment in terms of CAT score by a single experienced clinical assistant. The adverse events and the serious adverse events were also recorded.
RESULTS:
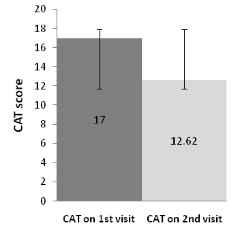
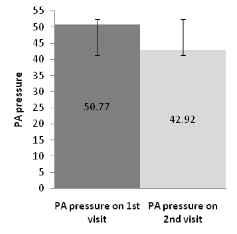
The project was initiated on 2nd week of January, 2013 and by the end of December, 2013, a total of 145 patients were prescribed sildenafil of which 81 patients completed the follow up at 12 weeks after starting the anti PH therapy. Out of the total number, 18 patients dropped out for various reasons (six for headache and seven for pedal edema, three for uneasiness and two for increase in breathlessness). One patient stopped the treatment for unknown reason. 45 of the patients are yet to complete the visit after 12 weeks. The table 1 elaborates the spirometric lung function values, the quality of life in terms of CAT score, the pulmonary artery systolic pressure (in Doppler-echocardiography), the adverse events and other parameters been listed under the common etiological headings. When a patient had more than one possible reason for having PH, the predominant one as per the investigator has been listed. Incidentally, we could get a repeat doppler-echo study been done in 13 patients observing a common protocol by the same echocardiographist; the result showed lowering of PAP concomitant to the lowering of the CAT score (figure 2). None of the patients had any previous exposure to sildenafil.
| |
All |
COPD |
DPLD |
Asthma |
H/o PTB |
OSA |
Miscellaneous* |
Indeterminate |
| No. of |
81 |
29 |
11 |
9 |
17 |
1 |
3 |
11 |
| patients |
| |
|
|
|
|
|
|
|
| Age |
62.43 ± |
65.24 ± |
58.36 ± |
63.11 ± |
59.82 ± |
74 |
69.67 ± 2.08 |
59.55 ± 10.21 |
| 10.17 |
7.47 |
8.63 |
14.33 |
12.13 |
| |
|
|
|
| CAT score |
15.33 ± |
15.28 ± |
16.09 ± |
15.56 ± |
14.18 ± |
19 |
15.33 ± 8.08 |
16 ± 4.58 |
| on 1stvisit |
5.52 |
4.5 |
8.1 |
6.46 |
5.57 |
| CAT score |
13.01 ± |
12.83 ± |
13.82 ± |
15 ± 7.05 |
12.29 ± |
11 |
9.33 ± 4.04 |
13.36 ± 5.77 |
| on 2ndvisit |
5.79 |
5.39 |
6.6 |
5.99 |
| p value |
0.004 |
0.03 |
0.23 |
0.43 |
0.17 |
- |
0.12 |
0.15 |
| (change in |
| CAT scores) |
|
|
|
|
|
|
|
|
| Resting |
93.77 ± |
93.56 ± |
89.8 ± |
95 ± 4.36 |
94.73 ± |
|
91 ± 9.64 |
95.36 ± 3.14 |
| saturation on |
95 |
| 1stvisit |
5.88 |
3.82 |
12.36 |
|
4.17 |
|
|
|
| Resting |
94.54 ± |
94.3 ± |
93.09 ± |
95.89 ± |
95.24 ± |
|
|
|
| saturation on |
97 |
94 ± 6.08 |
95.56 ± 3.05 |
| 3.79 |
3.46 |
5.05 |
2.03 |
2.95 |
| 2ndvisit |
|
|
|
| |
|
2.08 ± 2.7 |
1.6 ± 0.67 |
1.9 ± 0.87 |
1.69 ± |
1.88 ± |
1.46 ± 0.61 |
2.24 ± 0.61 |
| FVC(L) and |
|
(57.82 ± |
(55.09 ± |
(66.64 ± |
0.53 |
0.48 |
| |
(61.78 ± 37.81) |
(74.79 ± |
| % |
|
19.98) |
18.95) |
22.87) |
(54.65 ± |
(65.25 ± |
|
12.05) |
| |
|
|
|
|
17.51) |
13.48) |
|
|
| |
|
0.9 ± 0.45 |
1.4 ± 0.52 |
1.24 ± 0.59 |
1.11 ± |
1.26 ± |
1.16 ± 0.5 |
1.77 ± 0.51 |
| FEV1(L) |
|
(37.61 ± |
(59.39 ± |
(55.77 ± |
0.43 |
0.51 |
| |
(62.17 ± 42.33) |
(73.98 ± |
| and % |
|
17.58) |
17.02) |
21.22) |
(44.6 ± |
(57.5 ± |
| |
|
10.63) |
| |
|
|
|
|
16.37) |
26.96) |
|
| |
|
|
|
|
|
|
| %FEV1/FVC |
|
64.63 ± |
110.11 ± |
83.62 ± |
81.62 |
82.75 ± |
98.98 ± 9.67 |
97.44 ± 8.81 |
| |
17.83 |
14.97 |
22.37 |
±22.3 |
34.25 |
| |
|
|
|
| Initial PA |
47.11 ± |
46.66 ± |
47.4 ± |
44.09 ± 5.6 |
47.57 ± |
43.75 ± |
51.24 ± 11.19 |
48.43 ± 12.71 |
| pressure |
8.81 |
10.8 |
9.49 |
9.95 |
4.43 |
| Final PA |
42.92 ± |
|
|
|
|
|
|
|
| pressure |
7.82 |
|
|
|
|
|
|
|
| |
(n= 13) |
|
|
|
|
|
|
|
| AE |
19 |
7 |
2 |
6 |
1 |
0 |
1 |
2 |
| SAE |
15 |
5 |
2 |
3 |
3 |
0 |
0 |
2 |
* One bronchiectasis and two sarcoidosis
Table 1: The CAT score and the spirometric status (post bronchodilator) of the patients of PH been included for treatment with sildenafil (with. the standard deviation for the applicable parameters have been provided with ± values).
|
(A)
|
(B)
|
Figure 2: Comparison between initial and final CAT score in fig I(a) and pulmonary artery pressure in figure 1(b) of PH patients (n=13) having a repeat echo-doppler study after 12 weeks of treatment with sildenafil.
DISCUSSION:
There have been two important outcomes from the study. The first being that COPD remains the commonest cause of PH (35.8%) to pulmonologist in referral practice and that a wide spectrum of different conditions are responsible for class III PH in our part of the country. Roughly 29 % of the patients etiologically belong to asthma and possibly to suffering from tuberculosis in past together. This remains new as an information as these two conditions are not given a place in the international classification of PH (12). Looking at the lung function, the COPD patients appear to have severe disease (FEV1/FVC = 64.63 and % of FEV1 being 37.61± 17.58) while the asthmatics have relative milder disease (FEV1/FVC = 83.62 and % of FEV1 being 55.77±21.22) suggesting that the chronic asthmatics turning COPD phenotype by lung function are the unlikely members in the list. This makes the story more interesting to look for the pathogenesis of PH in our asthmatics. Roughly 21 % of the patients had history of tuberculosis in the past; this co-incidental finding lead us to separate these patients in a new group; they manifest a restrictive lung function as DPLD having a similar FVC (55 % vs. 55 %) compared to DPLD. Although reported, tuberculosis is also not a well documented and recognized entity to cause PH (13, 14). We could not find out the cause in 13.5 % of cases; surely we missed many conditions as the protocol was some-what restricted for logistic reasons. It is possible that one or more patients in this group belong to PAH.
The second important information derived from out observation is that there has been a universal and statistically significant (p=0.004) improvement in QoL in all the patients as a group. However, the change has been different in PH patients with different etiologies and when seen individually with different number of patients in each subgroup, despite being universal, the improvement is significant statistically only in COPD patients. The drug has been well tolerated with a total of 19 adverse events (AE), 14 hospitalizations from unrelated cause (not related to sildenafil) of which one succumbed. One very sick patient died at home before hospitalization. The common adverse events were pedal swelling, headache, initial increase in the SOB, and uneasiness with vague chest discomfort.
There may be questions about a) diagnosis of PH, b) Indication of therapy, c) dose and choice of the drug, d) The assessment tool. We admit that we had to deviate a lot from the guideline recommendations that included RHC universally for diagnosis. Our argument takes into account the available evidences for the diagnosis of PH from chest x-ray (PA view) and HRCT chest; these evidences have strong specificity for the presence of pulmonary hypertension. (7, 8, 9, 10) this was further supported by echocardiographic diagnosis of PH. Such diagnosis based on clinic-radio-echocardiographic criteria implies that the presence of PH is certain in our patients though the assessment of the exact pulmonary artery pressure is not possible. (15)
The next argument evolves an ethical issue to treat patients without RHC data as no guideline accepts the diagnosis of PH without RHC. To us, withholding the administration of anti-PH therapy cannot be justified any longer especially for people who are sick enough (WHO functional class III or IV) despite the optimum treatment of the underlying conditions. These issues had been discussed at the time of presentation to the Ethics Committee meeting where we could convince the members regarding our stand to remain humane in treating these patients on a defined real world protocol in logistically constraint circumstances when RHC is not available, not possible, or denied by the patients provided the candidates forward a proper informed consent.
There may be questions regarding the duration of optimum therapy for the underlying diseases. We took a cut off value of 2 weeks (except for very sick patients with obvious corpulmonale). To us it appeared that further delay may jeopardize the purpose of such treatment and it also looked unlikely for a patient to show at least the beginning of improvement further on optimum treatment of the underlying condition beyond this period. The next question involved was the treating agent and the dose. We had chosen sildenafil (a phosphodiesterase-5 inhibitor) as is used widely elsewhere and has been easily available with a relatively low cost in the market. We have kept the dose fixed for comparison; although further hiking the dose in some patients could have yielded a better result. The incorporation of the history of pulmonary tuberculosis in the etiological classification of Class III PH is a new addition in the list of etiologies.
Although tuberculosis has not been officially recognized in the guidelines as a cause of PH, we have shown that these patients form a good bulk (21%) of the PH population in our practice (16) and such patients are also recorded elsewhere.
Regarding assessment of a patient of PH, right heart catheterization and hemodynamic data appear important but are not mandatory as per the guideline recommendations. Tests like six minutes walk test, cardiopulmonary exercise testing, universal repeat echocardiography could have been worthwhile adjuncts to CAT score. Incidentally repeat echocardiography was possible in 13 of our patients concomitant to the repeat recording of CAT score . The observed echocardiographic improvement in terms of the measured PAP (systolic) has been found to go parallel to the improvement in CAT score (figure 2). For logistic reasons we could not measure anything else but CAT score. This is a validated instrument to measure the health status of the COPD patients, (17) and it has also been used in DPLD successfully. (18) Till date, there has been no data available regarding its use in OSA, or other lung conditions causing shortness of breath with jeopardy in lung function. We have chosen CAT for its simplicity, our expertise in using the instrument, and to maintain uniformity in recording the health status in several conditions. The number of patients been observed is small and it is difficult to compare the effect of sildenafil between the different etiological subgroups although it appears from the results that the effect is positive in all the etiological categories.
Despite the weaknesses been mentioned it appears that the treatment of symptomatic class III PH patients with sildenafil remains helpful in terms of improvement in the QoL. Prima face, the proposed clinic-radio-echocardiographic criteria appears acceptable although it needs validation before widespread recommendations. Further studies are urgently warranted in these directions. We feel it necessary for the medical intelligentsia to appreciate and formulate guideline for diagnosis and treatment of class III PH in our country based on the feasibility of investigations in face of resource constraints.
REFERENCE:
1. Seeger W, Adir Y, Barbera J A, Champion H, Coghlan J G, Cottin V, Marco T D, Galie N, Ghio S, Gibbs S, Martinez F J, Semigran M J, Simonneau G, Wells A U, Vachiery J L.
Pulmonary Hypertensionin Chronic Lung Diseases. J Am Coll Cardiol. 2013;62:D109-16.
2. Arias M A, Garcia-Rio F, Alonso-Fernandez A, Martinez I, Villamor J. Pulmonary hypertension in obstructive sleep apnoes: effects of continuous positive airway pressure. European Heart Journal (2006) 27, 1106-1113.
3. Studer, S M, Migliore, C. Quality of Life in PAH: Qualitative Insights From Patients and Caregivers. Advances in Pulmonary Hypertension. 2012; 10, 4: 222-226.
4. Galie N, Hoeper M M, Humbert M, Torbicki A, Vachiery J L, et al. Guidelines for the diagnosis and treatment of pulmonary hypertension: the Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS), endorsed by the International Society of Heart and Lung Transplantation (ISHLT). Eur Heart J 2009; 30: 2493–2537.
5. Mc Laughlin V V, Park M H, Rosenson R S, Rubin L J, Tapson V F, Vagre J. ACCP/AHA: 2009 Expert Consensus Document on Pulmonary Hypertension. Jr A. Col Cardiol 2009; 35:14, 1573- 1619
6. Saha D, Bhattacherjee P D, Das S K, Dey R, Ghosh M, Dutta I, Sarma M, Ghosh A, Bhattacharyya PS. Group III Pulmonary Hypertension: relative frequency of different etiologies in a referral pulmonary OPD. Pulmo Face, 2013:13, 3-8 (non indexed journal ISSN no. 2347 – 4823).
7. Kanemoto N, Furuya H, Etoh T, Sasamoto H, and Matsuyama S. Chest roentgenograms in primary pulmonary hypertension. Chest, 1979: 76, 45 – 49
8. Bush A, Gray H, Denison D M. Diagnosis of pulmonary hypertension from radiographic estimates of pulmonary arterial size. Thorax 1988; 43:127-131.
9. Tan R T, Kuzo R, Goodman L R, Siegel R, Hassler G B, Presberg K W. Utility of CT scan evaluation for predicting pulmonary hypertension in patients with parenchymal lung disease. Medical College of Wisconsin Lung Transplant Group. Chest 1998; 113(5): 1250–1256.
10. Ng C S, Wells A U, Padley S P. A CT sign of chronic pulmonary arterial hypertension: the ratio of main pulmonary artery to aortic diameter. J Thorac Imaging 1999; 14(4):270–278.
11. Rich S, ed. Executive Summary from the World Symposium on Primary Pulmonary Hypertension; September 6-10, 1998, Evian, France.
12. Simonneau G, Robbins I M, Beghetti, M et.al. Updated Clinical Classification of Pulmonary Hypertension. Journal of the American College of Cardiology, 2009:54, S43-54.
13. Patel V, Khaped K, Solanki B, Patel A, Rathod H, Patel J. Profile of pulmonary hypertension patients coming to civil hospital, Ahmedabad. Int J Res Med. 2013; 2 (1); 94-97.
14. Ahmed A E H, Ibrahim A S and Elshafie S M Pulmonary Hypertension in Patients with Treated Pulmonary Tuberculosis: Analysis of 14 Consecutive Cases. Circulatory, Respiratory and Pulmonary Medicine 2011:5 1–5.
15. Hammerstingl C, Schueler R, Bors L, Momcilovic D, Pabst S, et al. (2012) Diagnostic Value of Echocardiography in the Diagnosis of Pulmonary Hypertension. PLoS ONE 7(6): e38519. doi:10.1371/journal.pone.0038519.
16. Bhattacharyya P, Saha D, Bhattacherjee P D, Das S K, Bhattacharyya P P, Dey R. Tuberculosis and Pulmonary Hypertension: the results of a clinical observation. (Manuscript ID: "pvri_3_13". Send it to PVRI Journal as original article).
17. Jones P W, Harding G, Berry P et al. Development and first validation of the COPD Assessment Test. Eur Respir J 2009;34:648-654.
18. Tachikawa R, Otsuka K, Takeshita J, Tanaka K, Matsumoto T, Monden K. Evaluation of the chronic obstructive pulmonary disease assessment test for measurement of health-related quality of life in patients with interstitial lung disease. Respirology. 2012 Apr; 17(3):506-12. doi: 10.1111/j.1440-1843.2012.02131.x.
Dr. Parthasarathi Bhattacharyya
Consultant, Institute of Pulmocare and Research, Kolkata
Email: parthachest@yahoo.com